Guest Post: Diabetes Nerd Heaven!

This week I’ve been lucky enough to get an invitation to Diabetes UK’s Professional Conference. As a poor muggle with no medical training beyond half a century of trying to tame the beast that is our collective family blood sugar, it’s quite a privilege. And it’s also a huge privilege to be able to share it with the Arden’s Day Blog. I’m hoping that some information about what goes on between the doctors when they think we can’t see them will be a helpful for insight for JuiceBoxers in the UK and around the world.
This year’s 3 day conference is taking place in Livepool’s Exhibition Centre and Arena. We’ll be kicked out on Friday to make way for Eurovision. Apparently, King Charles and Queen Camillahave been down to have a look at the venue this morning. As far as I know, they didn’t stop in for any of the lecture sessions at the conference. That’s a shame – they’d have learned a lot! It’s a huge event, with 4 or 5 simultaneous presentations. It’s been an 11 hour day for me there, and I’m looking forward to Manchester City vs Arsenal and an early night before the sae again tomorrow.
So – to business, A huge part of this event is networking. Over 2,000 Consultants, Junior Doctors, Diabetes Specialist Nurses, Academics, Practice Managers and so on and so on gather in Liverpool to renew friendships and share their experiences informally. So far, I’ve only managed to create one awkward silence by revealing that I’ve no medical training. But neither have I been asked how I achieve an HbA1c of 39 (5.7 in US numbers). Make of that what you will.
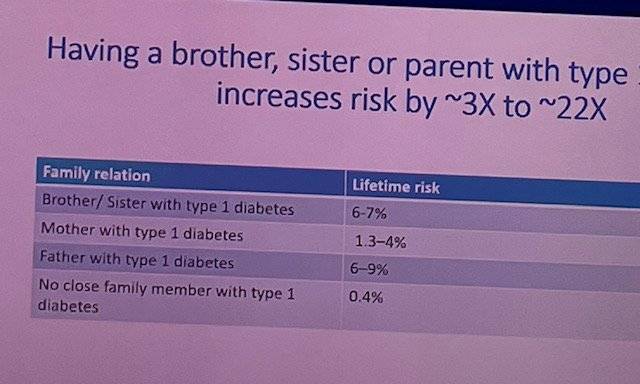
And I’ve learned! The first presentation of the conference was on “Nature or nurture” – the causation of diabetes. This comes up a lot as a question amongst us JuiceBoxers. Much of the chat was about Type 2 which is a really, really complicated question. For us Type 1’s Professor Ines Barrosso of Exeter University spoke of her research into the genes that are associated with Type 1. They’re now pretty clearly identified and partially explain this set of statistics:
The actual stats on family likelihood of developing T1, courtesy of Professor Barroso
But – and it’s a biggy – If one identical twin develops Type 1, there’s only a 40% chance that the other one will. And from that we can conclude that whilst there is a genetic component, there is also an environmental one. So it’s still your fault that you or your child lives with Type 1? You breast fed them, or not? You gave them anti-biotics or not? Nope. The “environmental factors” relating to causation of Type 1 are “largely unexplored” per Professor Barroso. What I take from that is that we cannot and must not blame ourselves, whether we have Type 1 or whether we have a child with Type 1. And that we need to support the research charities to find out what those causes are.
Type 2 is a different story. The impact of obesity is well understood. And there’s a genetic component. But for anyone who wants to say that one totally excludes the other – and this is the internet, we all know how it works – here’s a stat: The Pima Indians of Arizona and Mexico are the ethnic group with the highest incidence of T2 in the world, at 50%. But they’re a divided people. Those that live in Arizona, within the relative affluence and cheap calories of the USA, have rates above 50%, but their cousins in Mexico, in more straightened circumstances? 5%. The genes are playing their part, but so is lifestyle.
And other amazing things in brief:
• Get your doc or diabetes educator to give a talk in your child’s school. Not only will the kids learn something, but it’s a great way for kids who may not know each other to acknowledge each other as people living with Type 1. Having an ally in my year at school, or a couple of years above or below, would have gone a long way to addressing the loneliness I felt at school.
• Omnipod 5 really is coming to the UK. I can’t reveal when – because I don’t know exactly. But I can say that I won’t be ordering any more boxes of pods if I can get my healthcare team to switch me to a G6.
• Closed loop is coming as an “official” NHS supported tech in the UK. But don’t all rush for it at once. Rolling it out to every individual who may be eligible is going to take time.
• Dr Tabitha Randell of Nottingham University Hospital is a mega-star. Her patients are averaging an HbA1c in the 50s with minimal hypos. It won’t be a surprise to any JuiceBoxer that she’s a fan of getting a CGM on early and using a little bit more insulin, not a little bit less.
In terms of my wider experience of the HCPs, it’s become clear over the last 24 hours that the value of our “lived experience” is obvious to the clinical community. There are repeated statements about the need to listen to patients, ask what they want and ask how the medics can help. There’s real recognition, albeit with mixed levels of sensitivity, that the real experts in this condition are the people living with it. But… The Medical Establishment, like all great institutions, remains keen to look after itself before looking after the people it is supposed to serve. The word “safeguarding” is used in reference to patients, and deployed in a genuine effort to avoid damaging them. That’s great. But when it’s used to prevent those of us living with diabetes from damaging each other or ourselves it starts to be a bit weird. The internet exists. We sit alongside each other in clinics. We receive a monthly supply of a potentially lethal drug. We aren’t family pets that might or might not play nicely with other doggies. Peer support is coming as a pillar of care in the UK. It’s exciting. It requires clinicians to use judgement, tact and creativity to support it. From the guys I’ve met today, I think they’re going to be fine.
More tomorrow. Thanks for reading!
BOB
Rob (Bob Dee) Darbyshire
















Leave a comment