Iron rich foods: How to improve children’s iron status through diet

© 2009 – 2021, Gwen Dewar, Ph.D., all rights reserved
The smart consumption of iron rich foods
If your child has been diagnosed with an iron deficiency, it makes sense to examine his or her diet. But boosting iron levels isn’t just a matter of eating iron-rich foods.
Some foods contain iron, but they also contain compounds that decrease the body’s ability to absorb iron.
For instance, many grains, legumes, and vegetables contain phytates, chemical compounds which bind to iron.
Once bound together, these phytate-iron complexes can’t be digested by human enzymes in the gut — at least not if the pH of gut is in the neutral range. As a result, the iron you consume may end up passing through your body — unabsorbed (Petroski and Minich 2020).
In addition, tannins (found in tea, and in various fruits and vegetable foods) can inhibit iron absorption. So can certain proteins found in eggs.
So while we often hear that eggs and spinach are good sources of iron, the reality is more complicated. Experiments and laboratory analyses indicate that the iron in these foods is rather poorly-absorbed (Gordon and Chow 1984; Insel et al 2004; Ishikawa et al 2007).
Then there’s the problem of calcium and milk products.
Calcium competes with iron for absorption by the body (Insel et al 2004), so a calcium-rich meal can temporarily block iron absorption (Lönnerdal 2010).
And the effect may be amplified if a child consumes cow’s milk. In addition to calcium, cow’s milk contains a protein called alpha-casein that has an inhibitory effect on iron absorption (Kibangou et al 2005).
This may explain, at least in part, a well-known risk factor for iron deficiency in children: Kids who consume lots of cow’s milk are more likely to suffer from an iron deficiency (Uijterschout et al 2014; Gunnarson et al 2007; Hallberg 1998).
For example, in a study of Canadian children, toddlers were more likely to suffer from an iron deficiency if they were in the habit of consuming more than two cups of cow’s milk per day (Cox et al 2016).
What about young infants? They begin life on a diet of milk. How can babies avoid iron deficiency?
Babies are born with iron stores that help keep them remain iron-sufficient during the first few months postpartum.
And breast milk — despite its calcium content — is actually a good source of iron for infants. Although breast milk contains relatively low concentrations of iron (about 0.35 mg/L), it doesn’t contain the iron absorption inhibitor alpha casein.
Moreover, the iron in human breast milk comes in a form that is highly bioavailable, or easily-absorbed. In fact, researchers estimate that babies may be able to absorb anywhere from 45-100% of the iron in their breast milk (Qasem and Friel 2015).
However, by the time breastfed infants are 6 months old, their iron stores may be depleted. And the amount of iron they are getting from breast milk isn’t sufficient to keep up.
So researchers recommend that these babies begin consuming supplemental foods that are rich in iron (Qasem and Friel 2015).
Are there any foods that enhance iron absorption?
Yes. Vitamin C and “meat factor” (found in red meat, salmon, and other animal muscle proteins) help the body absorb iron and counteract the effects phytates.
In one study, adding 63 mg of vitamin C to a grain-based, iron-rich meal boosted iron absorption by almost 300% (Fidler et al 2009).
So what’s a good dietary strategy for boosting iron levels?
- Avoid the consumption of high levels of calcium (>40 mg) during meals that are intended to boost iron levels.
- Avoid other iron absorption inhibitors, like peppermint, chamomile, tea, and coffee.
- Encourage your child to consume iron-rich foods in combination with sources of vitamin C (like citrus fruits, peaches, papayas, sweet red peppers, berries, broccoli, and peas).
What kinds of iron-rich foods are appropriate for babies and toddlers?
Your baby’s first foods will be mashed-up. Pureed meats are rich in iron. Infants can also obtain some iron from non-meat sources — like mashed tofu, pureed green beans, strained peas, and pureed sweet potato. There are also iron-fortified cereals designed specifically for young infants.
As your child gets older, you can introduce more textured foods, but you will still need to be mindful of choking hazards.
For example, as I note in a table below, dried fruits are good sources of iron. But they should be avoided by babies and young toddlers, because can get stuck in a child’s throat.
For an evidence-based discussion of how to introduce solids, see this Parenting Science article.
What about meat? Do we have to eat meat to avoid iron deficiency?
Not if you are careful to get iron from other sources. But it’s worth noting that some families who avoid red meat may find it more difficult to maintain target iron levels.
For instance, in a study of more than 250 Israeli children, researchers found that kids who ate red meat rarely had a fourfold increased risk of being iron deficient (Moshe et al 2013). If you have concerns about iron deficiency and red meat isn’t on your menu, you may want to take special note of this evidence-based advice.
Which foods are especially rich in iron? How do different foods compare?
There are two classes of iron rich foods. Foods that contain heme iron, and foods that contain non-heme iron. Let’s take a closer look.
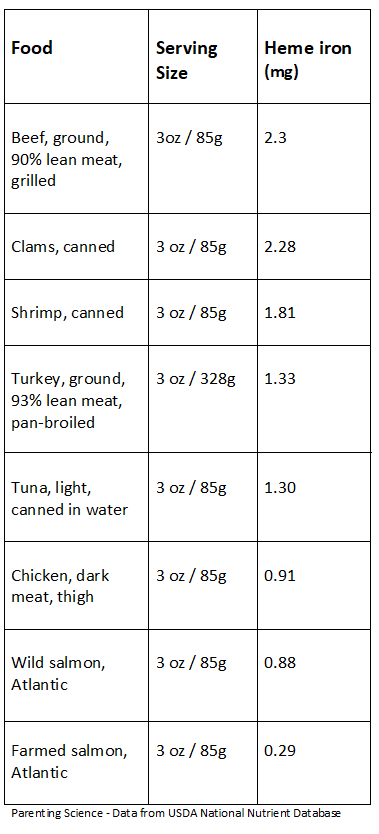
Iron rich foods: Sources of heme iron
Heme iron is the form of iron most easily absorbed by the body. It is found in animal muscle tissue. Here are some specific examples of heme iron rich foods, as rated by the USDA Nutrient Database.
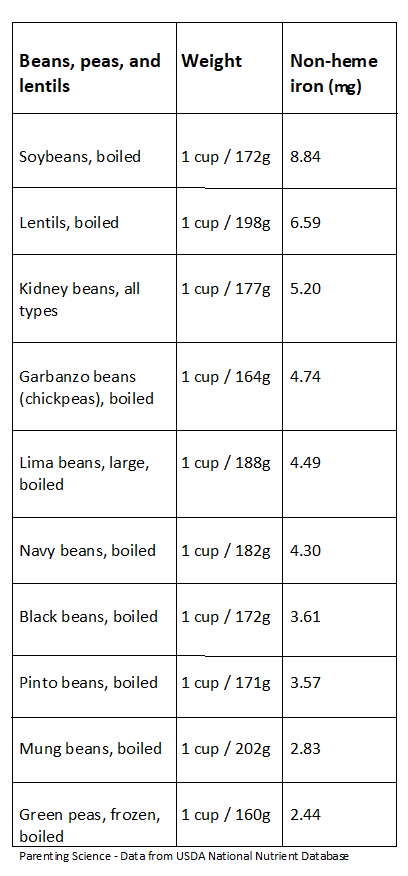
Iron rich foods: Sources of nonheme iron
Nonheme iron is found in plant foods, as well as in meat and eggs. Compared with heme iron, nonheme iron is much less efficiently absorbed.
Moreover, many sources of nonheme iron also contain phytates, which greatly reduce bioavailability. If you want to absorb significant quantities of nonheme iron, it’s especially important to combine it with vitamin C or meat. Again, see my article on iron absorption for more information.
I’ve created several charts with examples of nonheme, iron-rich foods. Both are compiled from information provided by the USDA Nutrient Database.
In this first chart, I highlight beans, peas, and lentils. Be aware that they pose a choking hazard to babies. You’ll want to mash them.
Tip for reducing phytates in these foods: Research suggests we can reduce phytate levels by cooking them for one hour at 95 degrees Celsius or 205 degrees Farenheit (Petroski and Minich 2020).
In addition, studies indicate that the regular consumption of fermentable fibers lowers the pH of the caecum, which can make it easier to absorb iron. Beans typically contain lots of fermentable fibers, so if you make a habit of eating beans, your body may absorb nonheme iron more efficiently (Petroski and Minich 2020).
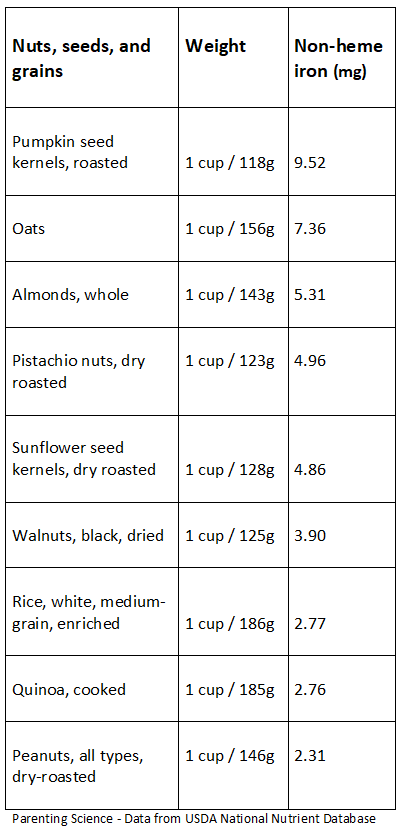
In this second chart, I highlight the nonheme iron content in some nuts, seeds, and grains. Once again, be mindful of choking hazards. Babies and younger toddlers shouldn’t consume nuts or seeds. And note that some children are allergic to tree nuts and/or peanuts, so you should consult your pediatrician about what foods are appropriate for your child.
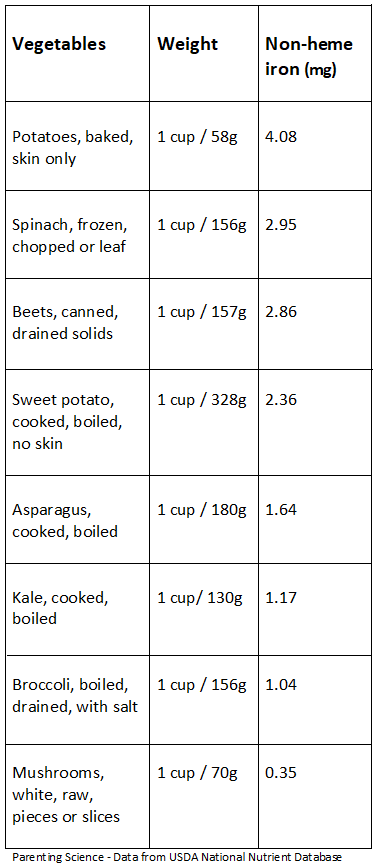
Finally, here are two charts highlighting a few fruits and vegetables. As always, be aware of choking hazards for babies and young toddlers. Dried fruits, for example, can get stuck in a child’s throat.

These tables represent only a small sampling of foods. For a more extensive listing of iron rich foods, check out the USDA Nutrient Database for yourself.
You can access as a PDF via this link.
References: Iron-rich foods
Bailey RL, Catellier DJ, Jun S, Dwyer JT, Jacquier EF, Anater AS, Eldridge AL. Total usual nutrient intakes of US children (under 48 months): findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr 2018;148:1557S–66S.
Cox KA, Parkin PC, Anderson LN, Chen Y, Birken CS, Maguire JL, Macarthur C, Borkhoff CM. 2016. Association Between Meat and Meat-Alternative Consumption and Iron Stores in Early Childhood. TARGet Kids! Collaboration. Acad Pediatr. 16(8):783-791.
Fidler MC, Davidsson L, Zeder C, and Hurrell RF. 2004. Erythorbic acid is a potent enhancer of nonheme-iron absorption. Am J Clin Nutr. 2004 Jan;79(1):99-102.
Gordon DT and Chao LS. 1984. Relationship of components in wheat bran and spinach to iron bioavailability in the anemic rat. Journal of Nutrition 114(3): 526-535.
Gunnarsson BS, Thorsdottir I,and Palsson G. 2007. Associations of iron status with dietary and other factors in 6-year-old children. Eur J Clin Nutr. 61(3):398-403.
Hallberg L. 1998. Does calcium interfere with iron absorption? Am. J. Clin. Nutr. 68: 3-4.
Insel, PM, Turner RE, and Ross D. 2003. Nutrition. 2nd edition.
Ishikawa SI, Tamaki S, Arihara K, Itoh M. 2007. Egg yolk protein and egg yolk phosvitin inhibit calcium, magnesium, and iron absorptions in rats. J Food Sci. 72(6):S412-9.
Kibangou IB, Bouhallab S, Henry G, Bureau F, Allouche S, Blais A, Guérin P, Arhan P, Bouglé DL. 2005. Milk proteins and iron absorption: contrasting effects of different caseinophosphopeptides. Pediatr Res. 58(4):731-4.
Moshe G, Amitai Y, Korchia G, Korchia L, Tenenbaum A, Rosenblum J, Schechter A. 2013. Anemia and iron deficiency in children: association with red meat and poultry consumption. J Pediatr Gastroenterol Nutr. 57(6):722-7.
Petroski W and Minich DM. Is There Such a Thing as “Anti-Nutrients”? A Narrative Review of Perceived Problematic Plant Compounds. 2020. Nutrients. 12(10):2929.
Qasem WA and Friel JK. 2015. An Overview of Iron in Term Breast-Fed Infants. Clin Med Insights Pediatr. 9:79-84.
Rutzke CJ, Glahn RP, Rutzke MA, Welch RM, Langhans RW, Albright LD, Combs GF Jr, and Wheeler RM. 2004. Bioavailability of iron from spinach using an in vitro/human Caco-2 cell bioassay model. Habitation (Elmsford). 10(1):7-1.
Uijterschout L, Vloemans J, Vos R, Teunisse PP, Hudig C, Bubbers S, Verbruggen S, Veldhorst M, de Leeuw T, van Goudoever JB, Brus F. 2014. Prevalence and risk factors of iron deficiency in healthy young children in the southwestern Netherlands. J Pediatr Gastroenterol Nutr. 58(2):195-200.
van der Merwe LF and Eussen SR. 2017. Iron status of young children in Europe. Am J Clin Nutr. 106(Suppl 6):1663S-1671S.
Content last modified 3/2021

















